Almost half of Americans take at least one prescription drug every month. Your body’s response to medications can vary greatly from others, which explains why drugs affect each person differently.
The CDC has found that adverse medication reactions send about 1.3 million people to emergency rooms each year – that’s one in every 250 Americans. These cases often stem from the body’s unique way of processing medications. Several factors affect how drugs are absorbed: the way they’re given, their form, and even your diet. The patient’s age also affects drug metabolism, and older people’s bodies tend to process medications more slowly.
A medication’s bioavailability – the amount that reaches your bloodstream – depends mostly on how you take it. Drugs given through IV lines have 100% bioavailability. Oral medications must survive both your digestive system and your liver’s first-pass metabolism. This process helps explain why some people respond quickly to certain medications while others take longer. This piece will explore how your body processes different medications and the key factors that influence drug absorption.
Mechanisms That Drive Drug Absorption
Drugs move from where they’re administered to the bloodstream through several distinct mechanisms that determine how quickly and completely they’re absorbed.
Passive Diffusion and the Role of Fick’s Law
Most drug molecules cross cell membranes through passive diffusion. Fick’s Law explains this process – the diffusion rate directly relates to concentration gradient, membrane surface area, and drug permeability coefficient, while being inversely related to membrane thickness. Drug molecules naturally move from high to low concentration areas without using energy.
Molecules that are small and dissolve in fat pass through membranes most easily, while larger or charged molecules struggle to cross. The small intestine’s extensive surface area, created by microvilli, significantly speeds up absorption. A drug’s ionization level plays a vital role – nonionized forms pass through membranes more easily than ionized forms.
Carrier-Mediated Transport: Active vs Facilitated Diffusion
Specialized carrier proteins help drugs that can’t cross membranes through passive diffusion alone. Facilitated diffusion uses carrier proteins that bind specific molecules and change shape. This allows substances to move along their concentration gradient without needing energy.
Active transport needs energy to push drugs against concentration gradients. Primary active transport directly uses ATP, while secondary active transport uses other solutes’ electrochemical potential. These processes become especially important for drugs that look like natural substances such as amino acids, peptides, and glucose.
Efflux Transporters: P-glycoprotein (P-gp) Limiting Absorption
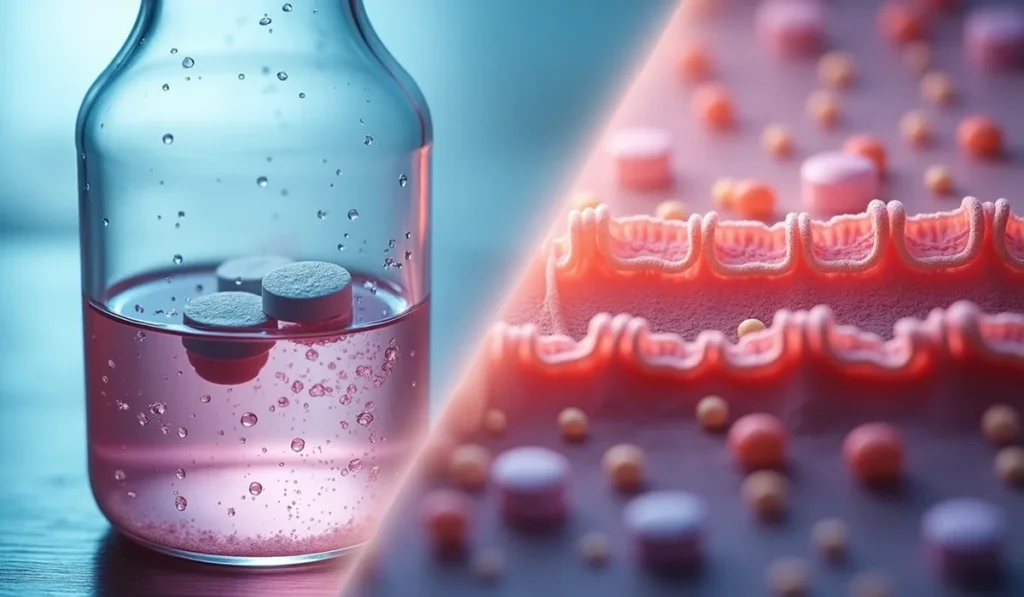
P-glycoprotein (P-gp) acts as a biological barrier by pushing drugs back into the intestinal cavity, which limits absorption. This ATP-powered pump exists mainly on intestinal epithelial cells’ outer surface.
P-gp affects many medications’ bioavailability, including anticancer drugs, calcium channel blockers, and HIV protease inhibitors. Its effect changes with drug concentration – high doses overwhelm P-gp transport, reducing its impact on overall absorption. Research with P-gp inhibitors shows this relationship clearly. The addition of P-gp inhibitor HM30181 boosted paclitaxel’s oral bioavailability from 3.4% to 41.3% in rats.
Drug-Specific Properties That Influence Absorption
Chemical and physical properties of a drug determine how well it enters your bloodstream and reaches its target. These core characteristics explain why some medications work faster than others and take hours to show their effects.
Solubility and Ionization: pKa and pH Interactions
pH-pKa interactions largely control how drugs spread across membranes. Most drugs work as weak acids or bases and exist in both ionized (hydrophilic) and non-ionized (lipophilic) forms at the same time. Cell membranes only allow non-ionized molecules to pass through passive diffusion, so the surrounding pH significantly changes absorption.
The acidic stomach environment helps weakly acidic drugs absorb better. Weakly basic drugs absorb more effectively in the small intestine’s higher pH environment. The Henderson-Hasselbalch equation governs this relationship by determining ionization state based on a drug’s pKa value and surrounding pH. When environmental pH changes from 6 to 8 for weakly basic drugs with pKa around 7, the unionized proportion jumps from 9% to 91%.
Particle Size and Surface Area Effect on Dissolution Rate
Dissolution rate relates inversely to particle size – smaller particles dissolve more quickly. A reduction in particle size creates more surface area for solvent interaction, which speeds up dissolution. Coenzyme Q10 studies clearly show this relationship. Nanocrystals of 80nm size improved bioavailability 7.3 times compared to coarse suspensions. The benefits plateau when particle size drops from 700nm to 120nm, with significant improvements only at 80nm.
Polymorphism and Crystalline Structure Variability
Different crystal forms (polymorphs) emerge from varying internal arrangements of drug molecules. These forms share similar chemical compositions but show different physical properties including:
- Solubility and dissolution rates
- Melting points and stability
- Mechanical properties that affect manufacturing
Metastable polymorphs usually show better solubility but might change to more stable, less soluble forms during storage. Chloramphenicol palmitate serves as a classic example – form B shows much better absorption and bioavailability than form A, which affects how well it works as medicine.
Dosage Form and Excipients: Tablets vs Solutions
Pharmaceutical formulation changes how quickly drugs absorb. Solutions enter the body faster than solid dosage forms that need to break down first. Tablets contain excipients that can help or slow down dissolution and absorption. Special coatings like enteric coating prevent dissolution until reaching specific areas, which controls where the body absorbs the drug.
Patient-Specific Factors Affecting Absorption Speed
Our body’s unique makeup determines how fast medicines work. These personal differences create major variations in how patients respond to treatments, unlike the consistent properties of drugs themselves.
Age-Related Changes in GI Physiology
Getting older changes how our body handles medications. Older patients produce less stomach acid and absorb less sugar, calcium, and iron. While digestion and movement stay mostly the same, the liver shrinks and gets less blood flow, which reduces its ability to process drugs. This means medicines like propranolol and labetalol, which the body usually processes before entering the bloodstream, become more available in older adults.
Gastric Emptying and Intestinal Transit Time
The small intestine absorbs most drugs because it has such a large surface area. This makes the stomach’s emptying speed a key factor in how quickly drugs get absorbed. Eating food, especially fatty meals, slows down this process. This slower movement can actually help some medicines work better. Metformin shows this effect clearly – when it stays in the stomach longer, the body absorbs more of it.
Food-Drug Interactions: Lipid vs Protein Meals
What you eat changes how well drugs work in your body. Fatty foods make it harder to absorb water-loving drugs but help fat-loving medicines dissolve better. Fats help drugs work better in several ways: they improve dissolution in digestive fluids, create tiny spaces for drugs that don’t mix well with water, and might reduce how much medicine gets broken down too early. Protein-rich meals can grab onto medicine ingredients and either block absorption or make them leave the body faster.
First-Pass Metabolism in Liver and Gut Wall
The body processes many medicines before they reach our bloodstream. Intestinal cells do more than just absorb – they contain powerful enzymes that break down drugs. CYP3A4 makes up about 80% of these intestinal enzymes. Even though gut enzymes only equal 1% of what the liver has, they affect drugs before the liver sees them. This explains why medicines like cyclosporine A, midazolam, and tacrolimus get broken down so much in the intestines.
Clinical Implications of Variable Absorption Rates
Drug delivery methods into the bloodstream play a crucial role in how well medications work and how safe they are. Medical professionals can create better treatment plans by understanding these effects on patients.
Bioavailability Differences by Route of Administration
Different administration routes change how much medication reaches the blood. Drugs rank from highest to lowest bioavailability: intravenous, rectal, oral, and topical. Intravenous medications achieve 100% bioavailability because they enter the bloodstream directly without needing absorption. This makes IV delivery the best choice during emergencies, with unconscious patients, or when medications need to work quickly.
Each delivery method reduces bioavailability differently. Oral medications offer convenience but face several absorption challenges. Transdermal patches deliver drugs slowly and steadily to the bloodstream while avoiding liver metabolism. Nasal or oral inhalation allows quick absorption through lung tissue, which also bypasses initial liver processing.
Absolute vs Relative Bioavailability in Drug Testing
Scientists use two main methods to review drug formulations. Absolute bioavailability looks at how well oral drugs work compared to their IV form, which shows absorption patterns. Relative bioavailability compares different versions of the same drug given the same way.
Generic drug makers must prove their products work within 80-125% of brand-name medications at a 90% confidence level to get FDA approval. This testing will give patients consistent results across different versions of their medications.
Therapeutic Window and Onset of Action Considerations
A drug’s therapeutic window shows the range where it helps without causing harm. Scientists calculate this by comparing the toxic dose affecting 50% of people (TD50) to the effective dose for 50% of people (ED50). Medications like warfarin, lithium, digoxin, and phenytoin need careful monitoring because they have narrow safety margins.
Absorption speed determines how quickly drugs start working. Emergency medications need quick absorption, while long-term conditions benefit from extended-release formulas. Drug effects also depend on where absorption happens. To cite an instance, acetaminophen absorbed in the upper small intestine might take longer to work if digestion slows down.
Conclusion
Drug absorption science explains why medications work differently for each person. These variations can be dramatic, even among people who seem similar. Healthcare providers and patients need to understand these differences. Your medication’s effectiveness depends on how its physical properties interact with your body’s unique systems. Several mechanisms determine how much medication reaches your bloodstream – passive diffusion, carrier-mediated transport, and efflux transporters all play their part.
Your body’s response to medications changes based on personal factors. As you age, your stomach produces different amounts of acid and processes drugs differently. What you eat can speed up or slow down how quickly your stomach empties. It can also help or block drug absorption. The same pills you take daily might work differently just because of your breakfast choices.
These variations in drug absorption directly shape how well treatments work. Each way of taking medication – whether by mouth, injection, or other methods – delivers different amounts of drug to your system. The concept of therapeutic windows shows why getting the right amount matters. Too little medication won’t help, while too much could harm you.
This understanding helps doctors and patients make better choices. Doctors can pick the right drug forms based on what works best for you. Patients learn why they need to take certain medications with food or on an empty stomach. Next time you take medicine, think about its remarkable path through your body and what makes it work. As pharmaceutical science advances our knowledge of these processes, medications become safer and more effective for everyone.